DGBI/FGIDs
Disorders of Gut-Brain Interaction (DGBI), also known as functional gastrointestinal disorders (FGIDs)
A. Esophageal Disorders
A1. FUNCTIONAL CHEST PAIN
Diagnostic criteria* Must include all of the following:
- Retrosternal chest pain or discomfort**
- Absence of associated esophageal symptoms, such as heartburn and dysphagia
- Absence of evidence that gastroesophageal reflux or eosinophilic esophagitis is the cause of the symptom
- Absence of major esophageal motor disorders†
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis with a frequency of at least once a week
**Cardiac causes should be ruled out
†Achalasia/EGJ outflow obstruction, diffuse esophageal spasm, jackhammer esophagus, absent peristalsis
A2. FUNCTIONAL HEARTBURN
Diagnostic criteria* Must include all of the following:
- Burning retrosternal discomfort or pain
- No symptom relief despite optimal antisecretory therapy
- Absence of evidence that gastroesophageal reflux** or eosinophilic esophagitis is the cause of the symptom
- Absence of major esophageal motor disorders†
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis with a frequency of at least twice a week
**Elevated acid exposure time and/or symptom reflux association
†Achalasia/EGJ outflow obstruction, diffuse esophageal spasm, jackhammer esophagus, absent peristalsis
A3. REFLUX HYPERSENSITIVITY
Diagnostic criteria* Must include all of the following:
- Retrosternal symptoms including heartburn and chest pain
- Normal endoscopy and absence of evidence that eosinophilic esophagitis is the cause of the symptoms
- Absence of major esophageal motor disorders**
- Evidence of triggering of symptoms by reflux events despite normal acid exposure on pH- or pH-impedance monitoring†
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis with a frequency of at least twice a week
**Achalasia/EGJ outflow obstruction, diffuse esophageal spasm, jackhammer esophagus, absent peristalsis
†Response to antisecretory therapy does not exclude the diagnosis
A4. GLOBUS
Diagnostic criteria* Must include all of the following:
- Persistent or intermittent, non-painful sensation of a lump or foreign body in the throat with no structural lesion identified on physical examination, laryngoscopy, or endoscopy
- Occurrence of the sensation between meals
- Absence of dysphagia or odynophagia
- Absence of a gastric inlet patch in the proximal esophagus
- Absence of evidence that gastroesophageal reflux or eosinophilic esophagitis is the cause of the symptom
- Absence of major esophageal motor disorders**
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis with a frequency of at least once a week.
**Achalasia/EGJ outflow obstruction, diffuse esophageal spasm, jackhammer esophagus, absent peristalsis
A5. FUNCTIONAL DYSPHAGIA
Diagnostic criteria* Must include all of the following:
- Sense of solid and/or liquid foods sticking, lodging, or passing abnormally through the esophagus
- Absence of evidence that esophageal mucosal or structural abnormality is the cause of the symptom
- Absence of evidence that gastroesophageal reflux or eosinophilic esophagitis is the cause of the symptom
- Absence of major esophageal motor disorders**
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis with a frequency of at least once a week
**Achalasia/EGJ outflow obstruction, diffuse esophageal spasm, jackhammer esophagus, absent peristalsis
B. Gastroduodenal Disorders
B1. FUNCTIONAL DYSPEPSIA*
Diagnostic criteria**
- One or more of the following:
- Bothersome postprandial fullness
- Bothersome early satiation
- Bothersome epigastric pain
- Bothersome epigastric burning
AND
- No evidence of structural disease (including at upper endoscopy) that is likely to explain the symptoms
*Must fulfill criteria for B1a. PDS and/or B1b. EPS
**Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
B1a. Postprandial Distress Syndrome (PDS)
Diagnostic criteria* Must include one or both of the following at least 3 days a week:
- Bothersome postprandial fullness (i.e., severe enough to impact on usual activities)
- Bothersome early satiation (i.e., severe enough to prevent finishing a regular size meal)
No evidence of organic, systemic, or metabolic disease that is likely to explain the symptoms
on routine investigations (including at upper endoscopy)
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
Supportive criteria
- Postprandial epigastric pain or burning, epigastric bloating, excessive belching, and nausea can also be present
- Vomiting warrants consideration of another disorder
- Heartburn is not a dyspeptic symptom but may often co-exist
- Symptoms that are relieved by evacuation of feces or gas should generally not be considered as part of dyspepsia
- Other individual digestive symptoms or groups of symptoms (e.g., from GERD and IBS) may co-exist with PDS
B1b. Epigastric Pain Syndrome (EPS)
Diagnostic criteria* Must include one or both of the following symptoms at least 1 day a week:
- Bothersome epigastric pain (i.e., severe enough to impact on usual activities)
- Bothersome epigastric burning (i.e., severe enough to impact on usual activities)
No evidence of organic, systemic, or metabolic disease that is likely to explain the symptoms
on routine investigations (including at upper endoscopy).
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
Supportive criteria
- Pain may be induced by ingestion of a meal, relieved by ingestion of a meal, or may occur while fasting
- Postprandial epigastric bloating, belching, and nausea can also be present
- Persistent vomiting likely suggests another disorder
- Heartburn is not a dyspeptic symptom but may often co-exist
- The pain does not fulfill biliary pain criteria
- Symptoms that are relieved by evacuation of feces or gas generally should not be considered as part of dyspepsia
- Other digestive symptoms (such as from GERD and IBS) may co-exist with EPS
B2. BELCHING DISORDERS
Diagnostic criteria*
Bothersome (i.e., severe enough to impact on usual activities) belching from the esophagus or stomach
more than 3 days a week
B2a. Excessive Supragastric Belching (from esophagus)
B2b. Excessive Gastric Belching (from stomach)
Supportive criteria
- Supragastric belching is supported by observing frequent, repetitive belching
- Gastric belching has no established clinical correlate
- Objective intraluminal impedance measurement is required to distinguish supragastric from gastric belching
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
B3. NAUSEA AND VOMITING DISORDERS
B3a. Chronic Nausea Vomiting Syndrome (CNVS)
Diagnostic criteria* Must include all of the following:
- Bothersome (i.e., severe enough to impact on usual activities) nausea, occurring at least 1 day per week and/or one or more vomiting episodes per week
- Self-induced vomiting, eating disorders, regurgitation, or rumination are excluded
- No evidence of organic, systemic, or metabolic diseases likely to explain the symptoms on routine investigations (including at upper endoscopy)
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
B3b. Cyclic Vomiting Syndrome (CVS)
Diagnostic criteria* Must include all of the following:
- Stereotypical episodes of vomiting regarding onset (acute) and duration (less than 1 week)
- At least three discrete episodes in the prior year and two episodes in the past 6 months, occurring at least 1 week apart
- Absence of vomiting between episodes, but other milder symptoms can be present between cycles
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
Supportive remark
History or family history of migraine headaches
B3c. Cannabinoid Hyperemesis Syndrome (CHS)
Diagnostic criteria* Must include all of the following:
- Stereotypical episodic vomiting resembling cyclic vomiting syndrome (CVS) in terms of onset, duration, and frequency
- Presentation after prolonged use of cannabis
- Relief of vomiting episodes by sustained cessation of cannabis use
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
Supportive remark
May be associated with pathologic bathing behavior (prolonged hot baths or showers)
B4. RUMINATION SYNDROME
Diagnostic criteria* Must include all of the following:
- Persistent or recurrent regurgitation of recently ingested food into the mouth with subsequent spitting or remastication and swallowing
- Regurgitation is not preceded by retching
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
Supportive criteria
- Effortless regurgitation events are usually not preceded by nausea
- Regurgitant contains recognizable food which may have a pleasant taste
- The process tends to cease when the regurgitated material becomes acidic
C. Bowel Disorders
C1. IRRITABLE BOWEL SYNDROME
Diagnostic criteria*
Recurrent abdominal pain on average at least 1 day/week in the last 3 months, associated with two or more of the following criteria:
- Related to defecation
- Associated with a change in frequency of stool
- Associated with a change in form (appearance) of stool
* Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
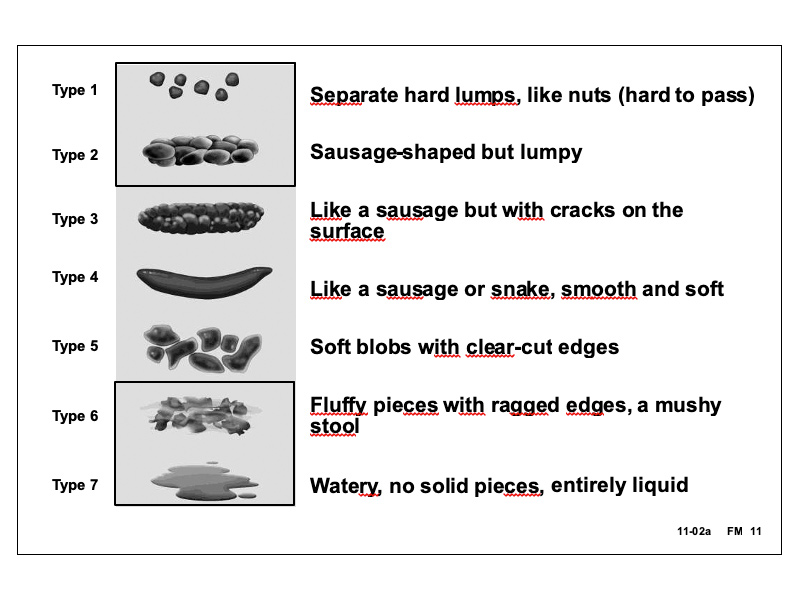
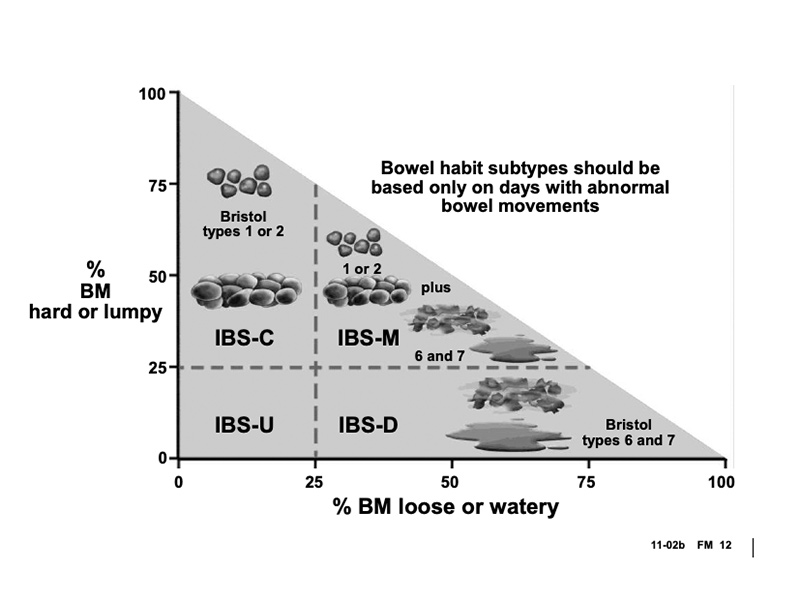
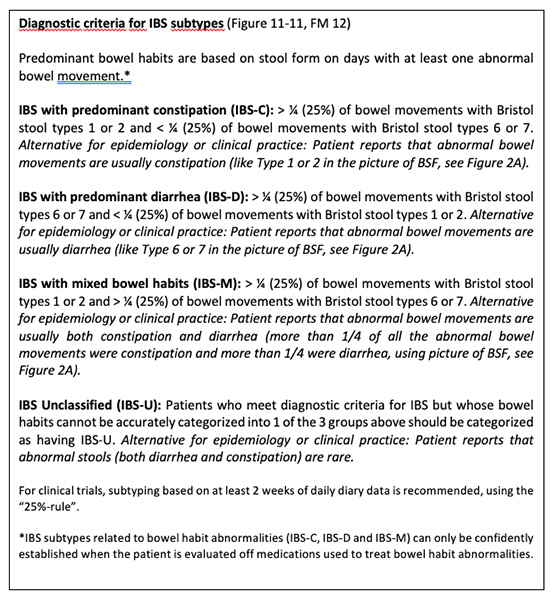
IBS Subtypes
C2. FUNCTIONAL CONSTIPATION
Diagnostic criteria*
- Must include two or more of the following:**
- Straining during more than ¼ (25%) of defecations
- Lumpy or hard stools (Bristol Stool Form Scale 1-2) more than ¼ (25%) of defecations
- Sensation of incomplete evacuation more than ¼ (25%) of defecations
- Sensation of anorectal obstruction/blockage more than ¼ (25%) of defecations
- Manual maneuvers to facilitate more than ¼ (25%) of defecations (e.g., digital evacuation, support of the pelvic floor)
- Fewer than three SBM per week
- Loose stools are rarely present without the use of laxatives
- Insufficient criteria for irritable bowel syndrome
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
**For research studies, patients meeting criteria for opioid-induced constipation (OIC) should not be given a
diagnosis of FC because it is difficult to distinguish between opioid side effects and other causes of constipation.
However, clinicians recognize that these two conditions may overlap.
C3. FUNCTIONAL DIARRHEA
Diagnostic criterion*
Loose or watery stools, without predominant abdominal pain or bothersome bloating, occurring in more than 25% of stools.**
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
**Patients meeting criteria for IBS-D (diarrhea-predominant IBS) should be excluded.
C4. FUNCTIONAL ABDOMINAL BLOATING/DISTENSION
Diagnostic criteria* Must include both of the following:
- Recurrent bloating and/or distension occurring on average at least 1 day/week; abdominal bloating and/or distension predominates over other symptoms.**
- There are insufficient criteria for a diagnosis of irritable bowel syndrome, functional constipation, functional diarrhea, or post-prandial distress syndrome.
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
**Mild pain related to bloating may be present as well as minor bowel movement abnormalities
C5. UNSPECIFIED FUNCTIONAL BOWEL DISORDER
Diagnostic criterion*
Bowel symptoms not attributable to an organic etiology that do not meet criteria for IBS,
or functional constipation, diarrhea or abdominal bloating/distension disorders
*Criterion fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
C6. OPIOID-INDUCED CONSTIPATION
Diagnostic criteria
- New, or worsening, symptoms of constipation when initiating, changing, or increasing opioid therapy, that must include two or more of the following:
- Straining during more than ¼ (25%) of defecations
- Lumpy or hard stools (Bristol Stool Form Scale 1-2) more than ¼ (25%) of defecations
- Sensation of incomplete evacuation more than ¼ (25%) of defecations
- Sensation of anorectal obstruction/blockage more than ¼ (25%) of defecations
- Manual maneuvers to facilitate more than ¼ (25%) of defecations (e.g., digital evacuation, support of the pelvic floor)
- Fewer than three SBM per week
- Loose stools are rarely present without the use of laxatives.
D. Centrally Mediated Disorders of GI Pain
D1. CENTRALLY MEDIATED ABDOMINAL PAIN SYNDROME*
Diagnostic criteria* Must include all of the following:
- Continuous or nearly continuous abdominal pain
- No or only occasional relationship of pain with physiological events (e.g., eating, defecation or menses)†
- Pain limits some aspect of daily functioning††
- The pain is not feigned
- Pain is not explained by another structural or functional gastrointestinal disorder or other medical condition
*CAPS is typically associated with psychosocial comorbidity, but there is no specific profile that can be used for diagnosis
**Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
†Some degree of gastrointestinal dysfunction may be present
††Daily function could include impairments in work, intimacy, social/leisure, family life, and caregiving for self or others
D2. NARCOTIC BOWEL SYNDROME/OPIOID-INDUCED GI HYPERALGESIA*
Diagnostic criteria* Must include all of the following:
- Chronic or frequently recurring abdominal pain* that is treated with acute high-dose or chronic narcotics
- The nature and intensity of the pain is not explained by a current or previous GI diagnosis**
- Two or more of the following:
- The pain worsens or incompletely resolves with continued or escalating dosages of narcotics
- There is marked worsening of pain when the narcotic dose wanes and improvement when narcotics are re-instituted (soar and crash)
- There is a progression of the frequency, duration, and intensity of pain episodes
*Pain must occur most days
**A patient may have a structural diagnosis (e.g., inflammatory bowel disease, chronic pancreatitis),
but the character or activity of the disease process is not sufficient to explain the pain
E. Gallbladder and Sphincter of Oddi Disorders
E1. BILIARY PAIN
Diagnostic criteria*
Pain located in the epigastrium and/or right upper quadrant and all of the following:
- Builds up to a steady level and lasts 30 minutes or longer
- Occurring at different intervals (not daily)
- Severe enough to interrupt daily activities or lead to an emergency department visit
- Not significantly (<20%) related to bowel movements
- Not significantly (<20%) relieved by postural change or acid suppression
Supportive criteria
The pain may be associated with:
- Nausea and vomiting
- Radiation to the back and/or right infra subscapular region
- Waking from sleep
E1a. Functional Gallbladder Disorder
Diagnostic criteria* Must include both of the following:
- Criteria for biliary pain*
- Absence of gallstones or other structural pathology
Supportive criteria
- Low ejection fraction on gallbladder scintigraphy
- Normal liver enzymes, conjugated bilirubin, and amylase/lipase
*Criteria for biliary pain: Pain located in the epigastrium and/or right upper quadrant and all of the following:
1. Builds up to a steady level and lasts 30 minutes or longer
2. Occurring at different intervals (not daily)
3. Severe enough to interrupt daily activities or lead to an emergency department visit
4. Not significantly (<20%) related to bowel movements
5. Not significantly (<20%) relieved by postural change or acid suppression
E1b. Functional Biliary Sphincter of Oddi Disorder
Diagnostic criteria* Must include all of the following:
- Criteria for biliary pain*
- Elevated liver enzymes or dilated bile duct, but not both
- Absence of bile duct stones or other structural abnormalities
Supportive criteria
- Normal amylase/lipase
- Abnormal sphincter of Oddi manometry
- Hepatobiliary scintigraphy
*Criteria for biliary pain: Pain located in the epigastrium and/or right upper quadrant and all of the following:
1. Builds up to a steady level and lasts 30 minutes or longer
2. Occurring at different intervals (not daily)
3. Severe enough to interrupt daily activities or lead to an emergency department visit
4. Not significantly (<20%) related to bowel movements
5. Not significantly (<20%) relieved by postural change or acid suppression
E2. FUNCTIONAL PANCREATIC SPHINCTER OF ODDI DISORDER
Diagnostic criteria* Must include all of the following:
- Documented recurrent episodes of pancreatitis (typical pain with amylase or lipase >3 times normal and/or imaging evidence of acute pancreatitis)
- Other etiologies of pancreatitis excluded
- Negative endoscopic ultrasound
- Abnormal sphincter manometry
F. Anorectal Disorders
F1. FECAL INCONTINENCE
Diagnostic criterion*
Recurrent uncontrolled passage of fecal material in an individual with a developmental age of at least 4 years
*Criterion fulfilled for the last 3 months. For research studies, consider onset of symptoms of at least 6 months previously with 2-4 episodes of FI over 4 weeks.
F2. FUNCTIONAL ANORECTAL PAIN
F2a. Levator Ani Syndrome
Diagnostic criteria* Must include all of the following:
- Chronic or recurrent rectal pain or aching
- Episodes last 30 minutes or longer
- Tenderness during traction on the puborectalis
- Exclusion of other causes of rectal pain such as inflammatory bowel disease, intramuscular abscess, anal fissure, thrombosed hemorrhoids, prostatitis, coccygodynia and major structural alterations of the pelvic floor
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
F2b. Unspecified Functional Anorectal Pain
Diagnostic criterion*
Symptom criteria for chronic levator ani syndrome but no tenderness during posterior traction on the puborectalis muscle
*Criterion fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
F2c. Proctalgia Fugax
Diagnostic criteria* Must include all of the following:
- Recurrent episodes of pain localized to the rectum and unrelated to defecation
- Episodes last from seconds to minutes with a maximum duration of 30 minutes
- There is no anorectal pain between episodes
- Exclusion of other causes of rectal pain such as inflammatory bowel disease, intramuscular abscess, anal fissure, thrombosed hemorrhoids, prostatitis, coccygodynia and major structural alterations of the pelvic floor
*For research purposes, criteria must be fulfilled for 3 months with symptom onset at least 6 months prior to diagnosis.
F3. FUNCTIONAL DEFECATION DISORDERS
Diagnostic criteria* Must include all of the following:
- The patient must satisfy diagnostic criteria for functional constipation and/or irritable bowel syndrome with constipation
- During repeated attempts to defecate, there must be features of impaired evacuation, as demonstrated by 2 of the following 3 tests:
- Abnormal balloon expulsion test
- Abnormal anorectal evacuation pattern with manometry or anal surface EMG
- Impaired rectal evacuation by imaging
*Criteria fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
Subcategories F3a and F3b apply to patients who satisfy criteria for FDD
F3a. Inadequate Defecatory Propulsion
Diagnostic criterion*
Inadequate propulsive forces as measured with manometry with or without inappropriate contraction
of the anal sphincter and/or pelvic floor muscles**
*Criterion fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
**This criterion is defined by age- and gender-appropriate normal values for the technique
F3b. Dyssynergic Defecation
Diagnostic criterion*
Inappropriate contraction of the pelvic floor as measured with anal surface EMG or manometry
with adequate propulsive forces during attempted defecation**
*Criterion fulfilled for the last 3 months with symptom onset at least 6 months prior to diagnosis
**This criterion is defined by age- and gender-appropriate normal values for the technique



Comments
Post a Comment